녹농균 감염 시장 크기 - 분석
USD 기준 시장 규모 Bn
CAGR8.6%
| 연구 기간 | 2025-2032 |
| 추정 기준 연도 | 2024 |
| CAGR | 8.6% |
| 시장 집중도 | Medium |
| 주요 플레이어 | 카테고리, 공장 투어, 머스크 & 공동., 인기 카테고리, Basilea 약학 및 기타 |
저희에게 알려주세요!
녹농균 감염 시장 트렌드
Market Driver - Novel Therapies에 대한 수요 상승 방지 감염
효과적으로 기존 항균성 암염을 가진 multidrug-resistant pseudomonas aeruginosa 감염을 대우하는 불안정성은 더 새로운 처리 paradigms를 위한 수요를 증가하기 위하여 지도했습니다. 전통적인 항생제는 이러한 "Superbugs"와 저항을 해결할 수있는 혁신적인 비 항생제 치료를위한 Dwindling 약물 파이프라인 통화에 대해 실패합니다. 또한, 크로스 저항 문제에 직면하지 않고 특히 Pseudomonas aeruginosa를 대상으로 할 수있는 새로운 약물을 개발해야합니다.
전통적인 작은 molecule 항생제는 지속적으로 진화 저항 메커니즘을 점점 증가시키는 것입니다. monoclonal 항체, 항 바이러스제, 바이오필름-disrupting 대리인과 같은 Novel 치료 접근은, phage 치료에는 최근 시간에 있는 뜻깊은 연구 관심사가 있습니다. 이 대안 modalities는 비 항생제 메커니즘을 통해 curb 세균성 병리를 목표로, 저항의 출현을 느리게.
몸의 자연 방어를 활용한 Immunotherapies도 탐구되고 있습니다. Monoclonal antibodies는 virulent 균주에 대한 보호에 잠재적으로 매력적인 면역 접근 방식을 나타냅니다. Pseudomonas aeruginosa의 중요한 virulence 요인을 표적하는 대리인은 유형 III 분비 체계 및 관련 독소 파악 약속을 좋아합니다.
또한, 약물 클래스 사이의 synergies를 레버링하는 조합 요법은 내성 변형에 대한 항균 활동을 복원 할 수있는 능력을 보여줍니다. phage endolysins, bacteriophage 치료를 포함한 대체 요법 및 설계 된 synergy는 낙관 최적화를 생성하고 있습니다.
Market Opportunity - Antibiotics에 대안으로 Bacteriophage Therapies에 초점 증가
Pseudomonas aeruginosa 감염 시장에 있는 1개의 promising 기회는 전통적인 항생제에 대안으로 bacteriophage 치료법을 개발하는 것에 집중합니다. Bacteriophages는 인간 세포를 해치지 않고 특정 박테리아 균류를 선택적으로 표적하고 죽이는 바이러스입니다.
자체 검사 능력으로 인해 phage therapies는 크게 관련 연구 및 제조 비용을 낮추기 위해 새로운 항생 개발에 직면 한 많은 도전을 극복 할 수 있습니다. 몇몇 생명 공학 및 약제 회사는 지금 P. aeruginosa 같이 어려운 감염을 위한 phage 치료에 임상 시험을 지휘하고, 다른 항생 저항하는 긴장에 customizable 생활 약으로 그들의 잠재력을 격려했습니다.
더 많은 증거는 항생제와 비교된 그들의 안전 그리고 효능에, phage 치료는 P. aeruginosa 및 다른 multidrug 저항하는 병원균을 위한 새로운 처리 선택권을 열 수 있었습니다. 각자 침투하는 그들의 능력은 또한 더 세균성 저항을 모는 선택적인 압력을 완화합니다. 지속적인 연구가 계속 그들의 약속을 검증하는 경우에, bacteriophage 치료는 항생 저항에 대하여 우리의 지속적인 전투에서 돌파할지도 모릅니다.
처방자의 선호도 녹농균 감염 시장
Pseudomonas aeruginosa는 급성 및 만성 폐 감염을 일으킬 것으로 알려진 opportunistic 병원체입니다. 치료는 일반적으로 항균 약의 조합을 포함, 선택과 함께 단계와 감염의 심각성.
온건한 심각한 감염에 온화한을 위해, ciprofloxacin (Ciprobay) 또는 levofloxacin (Tavanic)와 같은 fluoroquinolone를 가진 monotherapy는 수시로 첫번째 선입니다. 더 심각한 케이스는 일반적으로 tobramycin (Nebcin)와 같은 아미노글리코사이드와 함께 piperacillin-tazobactam (Zosyn)와 같은 베타 락탐을 결합하는 이중 치료가 필요합니다. Chronically 감염된 환자는 colistin methanesulfonate (Coly-Mycin M)와 같은 anti-pseudomonal 약의 흡입 된 정립을 처방 할 수 있습니다.
감염이 진행되고 더 저항하는, 조합 IV 치료는 호의를 받습니다. 인기 옵션은 beta-lactam / beta-lactamase 억제제 조합을 포함 - 예를 들어, ceftazidime (Fortaz) avibactam (Avycaz) - 또는 imipenem-cilastatin (Primaxin)와 같은 carbapenem. 마지막 선 multidrug 저항은 수시로 levofloxacin (Arikayce) 또는 polymyxin 항생제 aztreonam (Cayston) 같이 더 새로운 inhaled 항생제의 사용에 지도합니다.
선택에 영향을 미치는 다른 요인은 환자의 comorbidities, 규정 준수 역사, 감염 사이트 (예 : 상처 vs. 폐) 및 개별 병원성 약 저항 패턴에 대한 문화 / 민감성 테스트 결과가 포함되어 있습니다. 치료 응답 및 저항 발달의 가까이에 또한 드라이브 처방전의 순차적인 치료 결정.
치료 옵션 분석 녹농균 감염 시장
Pseudomonas Aeruginosa 감염은 환자의 면역 상태와 감염의 위치에 따라 온화한에서 심한 범위 수 있습니다. 치료는 표적 항균 치료 및 관련 위험 요인의 통제를 포함합니다.
온화한 감염을 위해, ciprofloxacin 또는 levofloxacin와 같은 구두 항생제는 첫번째 선 선택권입니다. 그들은 호흡기 및 urinary 트랙터 사이트에서 적절한 농도를 달성합니다. 그러나, 저항은 수시로 더 강한 대리인을 요구하는 빨리 발전합니다.
더 심각한 감염은 multidrug 저항하는 Pseudomonas 긴장을 포함합니다. 첫번째 정맥 선택권은 보통 piperacillin-tazobactam 조합입니다. 그것의 넓은 스펙트럼 및 살균 활동은 Pseudomonas를 포함하여 다양한 그램 부정 막대에 대하여 효과적입니다.
piperacillin-tazobactam 또는 가혹하게 ill 환자에 저항하는 감염을 위해, 선택의 처리는 imipenem 또는 meropenem 같이 antipseudomonal carbapenem입니다. 많은 저항하는 긴장에 대하여 이 administer 믿을 수 있는 적용. Cefepepime는 대안 그러나 저항은 최근에 증가되었습니다.
체계적인 치료를 받을 수 없는 환자를 위해 또는 만성 폐 감염이, 흡입된 tobramycin는 유익합니다. 감염 위치에 그것의 높은 노출량은 다른 약의 빈 조직 침투를 극복하는 것을 돕습니다. aminoglycoside를 가진 antipseudomonal 대리인을 사용하는 조합 치료는 또한 생활 threatening 상황에서 시도될지도 모릅니다.
주요 플레이어가 채택한 주요 승리 전략 녹농균 감염 시장
R&D를 통한 제품 혁신: 신약 개발 및 치료 옵션은 기업이 경쟁 업체에 가장자리를 얻고 더 많은 시장 점유율을 캡처하는 데 도움이되었습니다. 예를 들어 Merck는 2014 년 SIVEXTRO (tedizolid phosphate)를 출시했으며 급성 세균성 피부 및 피부 구조 감염의 치료에 대한 최초의 oxazolidinone 항균 승인을 받았습니다.
전략적 인수: 회사는 보완 자산 및 기술로 회사의 전략적 인수를 통해 제품 파이프라인 및 시장 위치를 강화했습니다. 예를 들어, 2018에서 Pfizer는 BRAF 억제제 BRAFTOVI를 포함한 표적 암 의약품의 파이프라인에 액세스 할 수있는 Array BioPharma를 인수했습니다.
파트너십 및 라이센스 거래: Biotech사와의 파트너쉽을 맺고 개발 비용과 위험을 공유합니다. 2019 년 Novartis는 ETX2514를 개발하기 위해 Entasis Therapeutics와 협력을 체결했습니다. 새로운 고정 복용량 조합 항균 약.
새로운 시장의 초점: 시장 잠재력, 기업은 아시아, 아프리카 및 라틴 아메리카의 높은 성장에 초점을 맞추고 현지 제조 및 마케팅 파트너십을 통해. 예를 들어, AstraZeneca는 중국의 자회사를 설립하고 제조 및 흡입 항생 Tobramycin을 배포하기위한 여러 로컬 약국 회사와 협력했습니다.
세그먼트 분석 녹농균 감염 시장

Insights, 관리 루트 : 구강 루트 드라이브 시장 환자 준수 및 편의성에 의해 주도
행정의 경로에서, 구두 행정은 2024년에 시장의 50.4% 몫을 위해, 더 나은 환자 합격 및 수락을 owing 예상됩니다. 만성 P. aeruginosa 감염 대우는 항균 약의 장기 행정을 요구합니다. 구두 경로는 이 상황에 있는 보호자 약에 명백한 이점을 제공합니다, 구두 약은 더 적은 invasive, 자기administer에 더 편리한 및 환자의 일상적인 일상 생활에서 잘 적응시킵니다. 이것은 크게 치료 요법을 준수합니다.
구두 약은 또한 in-hospital intravenous therapies와 반대로 외래 배려를 허용합니다. 의료 시스템에 대한 부담을 완화하고 전반적인 비용 절감. 제약 회사는 이러한 연구 및 개발 노력에 초점을 맞추고 새로운 구두 항-pseudomonal 약 및 정립을 개발하여 높은 성장 구두 세그먼트를 활용합니다.
추가 통찰력 녹농균 감염 시장
- Pseudomonas Aeruginosa는 전 세계적으로 병원 검사 감염의 상당한 비율을 담당합니다. pneumonia, UTI, 상처 감염의 주요 원인은 특히 immunocompromised 환자에서. 저항하는 긴장의 상승은 대우하기 위하여 가장 도전적인 감염의 한개 만들었습니다.
- Pseudomonas aeruginosa 감염의 상승한 우선권은, 특히 의료 관련 조정에서, 중요한 관심사입니다. 추정된 51,000 의료 관련 Pseudomonas aeruginosa 감염은 미국에서 발생합니다. 매년 새로운 치료법에 대한 수요에 크게 기여.
- Armata Pharmaceuticals와 Spexis는 Pseudomonas aeruginosa를 대상으로하는 치료 phages 및 항생제의 개발에서 업계의 초점을 반영합니다.
경쟁 개요 녹농균 감염 시장
pseudomonas aeruginosa 감염 시장에서 운영하는 주요 선수는 AstraZeneca, Pfizer, Merck & Co., Novartis, Basilea Pharmaceutica, Armata Pharmaceuticals, Spexis, AvidBiotics Corp, Polyphor AG 및 Phico Therapeutics를 포함합니다.
녹농균 감염 시장 선두
- 카테고리
- 공장 투어
- 머스크 & 공동.
- 인기 카테고리
- Basilea 약학
녹농균 감염 시장 - 경쟁 경쟁

녹농균 감염 시장
(주요 플레이어가 지배)
(많은 플레이어가 있는 매우 경쟁적)
최근 개발 녹농균 감염 시장
- 6 월 2024에서 Armata Pharmaceuticals는 Pseudomonas aeruginosa에 의한 호흡 감염을 대상으로 AP PA02의 Phase II 임상 시험을 완료했습니다. 결과는 cystic fibrosis 환자에 있는 promising efficacy, 잠재적으로 미래 처리 승인을 위한 방법을 포장합니다. 회사는 또한 최종 환자 후속이 8 월 2024에 예정되고 재판에서 최고 결과는 2024의 두 번째 반에서 사용할 것으로 예상됩니다. 이 시험은 비 경막한 Fibrosis Bronchiectasis (NCFB)를 가진 환자에 집중하는 다중 센터, 두 배 blind, placebo 통제된 학문, 흡입된 AP-PA02의 안전 그리고 효능을 평가하기 위하여 겨냥하는
- 3 월 2024에서 AstraZeneca는 Pseudomonas Aeruginosa의 다약 저항하는 긴장을 표적으로 하는 그것의 새로운 항생제의 단계 III 예심에서 긍정적인 결과를 발표했습니다, 두드러지게 병에 넣어진 환자에 있는 감염 내구를 감소시켰습니다. AstraZeneca는 항생제 및 항균성 관련 여러 협력 및 개발 노력에 참여하고 있습니다. 또한 Pfizer의 새로운 항생제 조합과 같은 항생 분야에서 지속적인 중요한 개발이 있습니다. 멀티drug-resistant Pseudomonas aeruginosa 및 기타 Gram-negative 박테리아는 이러한 감염에 중요한 새로운 치료를 제공 할 수 있습니다.
- 2023년 말에 Spexis는 Mirepavadin을 위한 단계 I 예심의 시작을 드러냈습니다, multi-drug 저항하는 Pseudomonas aeruginosa를 겨냥한 흡입된 항생제. 약은 cystic fibrosis와 bronchiectasis 환자에 있는 unmet 필요를 해결하기 위하여 예상됩니다. 단계 I 임상 시험은 건강 자원 봉사자에 있는 흡입된 murepavadin (iMPV)의 안전, tolerability 및 pharmacokinetics를 시험했습니다. 결과는 iMPV가 심각한 불리한 사건과 더불어 모든 복용량 수준에 잘 관용된다는 것을 보여주었습니다. 이 연구는 또한 폐 조직에 있는 효과적인 농도를 달성하고 낮은 체계적인 bioavailability를 유지하고, cystic fibrosis 환자에 있는 Pseudomonas aeruginosa를 표적으로 하기를 위해 근본적 인 것을 설명했습니다.
8 월 2023에서, Pfizer는 Pseudomonas Aeruginosa에 의해 일어난 병원 장비 감염을 대우하는 것을 목적으로 하는 새로운 항균 펩티드 치료를 발사했습니다. 이 치료는 세균성 저항 메커니즘을 대상으로 환자의 결과를 개선 할 것으로 예상됩니다. Pfizer는 Zavicefta (ceftazidime와 avibactam의 조합)와 같은 처리를 포함하여 병원 장비 감염을 위한 새로운 항균 치료 개발에 활동했습니다. Zavicefta는 Pseudomonas aeruginosa를 포함하여 다약 저항하는 그램 부정 박테리아에 기인한 심각한 감염을 대우하기 위하여, 특히 병원 aquired pneumonia의 경우에는 디자인됩니다.
녹농균 감염 시장 세분화
- 약으로
- 단일 클론 항체
- 작은 Molecule
- 사이트맵
- 행정구역
- 뚱 베어
- 교육과정
- 제품정보
- 감염
- 호흡 감염
- Urinary Tract 감염 (UTIs)
- 환자 유형
- 병원 문의 감염
- 커뮤니티 감염

구매 옵션을 알아보시겠어요?이 보고서의 개별 섹션?
Ghanshyam Shrivastava - 경영 컨설팅 및 연구 분야에서 20년 이상의 경험을 가진 Ghanshyam Shrivastava는 수석 컨설턴트로서 생물학 및 바이오시밀러에 대한 광범위한 전문 지식을 제공합니다. 그의 주요 전문 분야는 시장 진입 및 확장 전략, 경쟁 정보, 다양한 치료 범주 및 API에 사용되는 다양한 약물의 다각화된 포트폴리오에 걸친 전략적 전환과 같은 분야입니다. 그는 고객이 직면한 주요 과제를 파악하고 전략적 의사 결정 역량을 강화하기 위한 강력한 솔루션을 제공하는 데 능숙합니다. 시장에 대한 그의 포괄적인 이해는 연구 보고서 및 비즈니스 의사 결정에 귀중한 기여를 보장합니다.
Ghanshyam은 업계 컨퍼런스에서 인기 있는 연설자이며 제약 산업에 대한 다양한 출판물에 기고합니다.
자주 묻는 질문 :
어떻게 aeruginosa 감염 시장?
pseudomonas aeruginosa 감염 시장은 2024년에 USD 1.3 Bn에 평가되고 2031년까지 USD 2.28 Bn에 도달할 것으로 예상됩니다.
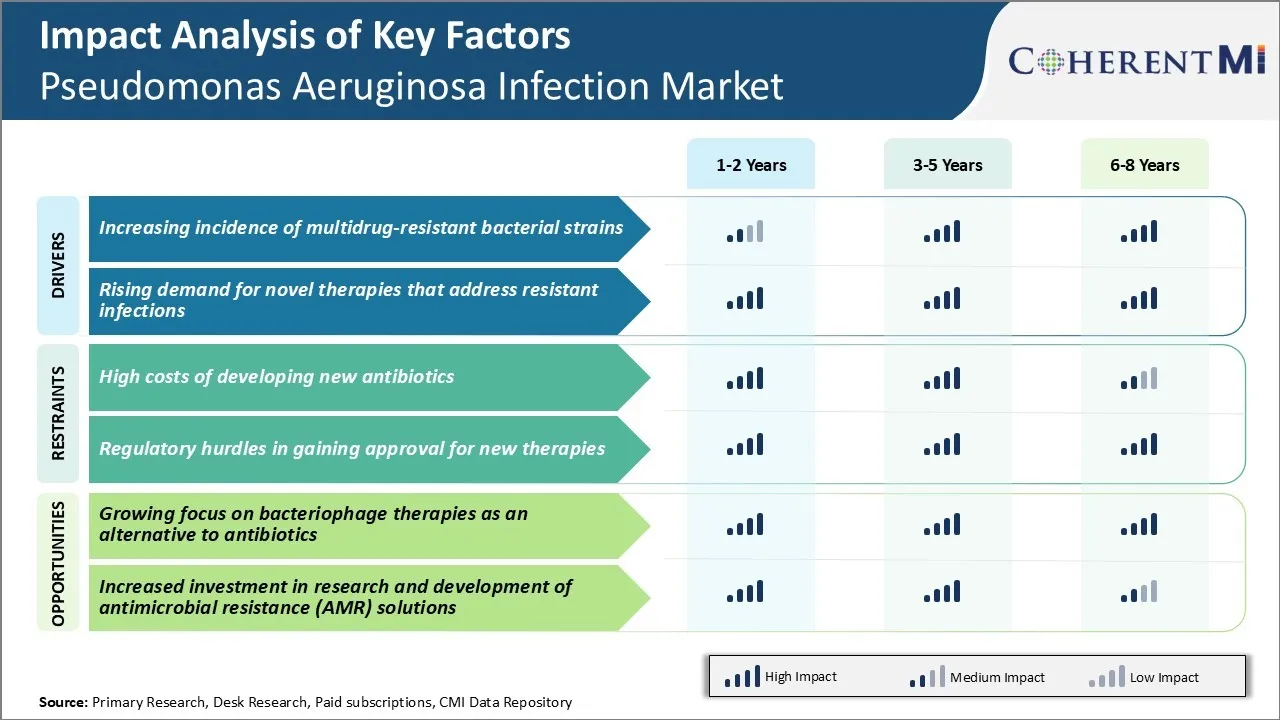
어떤 주요 요인은 pseudomonas aeruginosa 감염 시장의 성장?
새로운 치료에 대한 승인을 얻기 위해 새로운 항생제 및 규제 장애물 개발의 높은 비용은 주요 요인은 pseudomonas aeruginosa 감염 시장의 성장을 hampering.
pseudomonas aeruginosa 감염 시장 성장을 운전하는 주요 요인은 무엇입니까?
감염을 해결하는 새로운 치료에 대한 멀티 드루 저항하는 세균성 변형 및 상승 수요의 발생은 pseudomonas aeruginosa 감염 시장을 운전하는 주요 요인입니다.
pseudomonas aeruginosa 감염 시장에 있는 주요한 약은 무엇입니까?
주요한 약 세그먼트는 monoclonal 항체입니다.
pseudomonas aeruginosa 감염 시장에서 작동하는 주요 선수는 무엇입니까?
AstraZeneca, Pfizer, Merck & Co., Novartis, Basilea Pharmaceutica, Armata Pharmaceuticals, Spexis, AvidBiotics Corp, Polyphor AG 및 Phico Therapeutics는 주요 선수입니다.
pseudomonas aeruginosa 감염 시장의 CAGR 무엇입니까?
pseudomonas aeruginosa 감염 시장의 CAGR는 2024-2031에서 8.36%가 될 것으로 예상됩니다.