Spina Bifida In-Utero Market Trends
Market Driver - Increasing Awareness and Advancements in Prenatal Diagnosis Boosts Industry Developments.
With the advancements in medical technologies, prenatal diagnosis of spinal bifida has become more accessible than ever before. Fetal ultrasound scans and MRI have enabled physicians to identify spinal bifida in-utero with a high degree of accuracy even during early stages of pregnancy. Such screenings are now routinely offered to expecting mothers as part of standard prenatal care in many developed nations. This has significantly boosted early detection rates of spinal bifida and other neural tube defects before birth.
At the same time, various non-profit organizations and support groups related to spinal bifida have also intensified their efforts over the years to spread public awareness about its symptoms, risk factors, available screening options and treatment approaches. Their social media campaigns, seminars at schools and healthcare facilities have helped disseminate useful information to expecting mothers and the surrounding community. As a result of these combined efforts, many more women are now informed about the importance of undergoing spinal bifida screenings during pregnancy. Early diagnosis allows families to gain a thorough understanding of the condition and make well-prepared decisions regarding ongoing care of the child after birth.
At the clinical level as well, diagnostic techniques continue to evolve. No longer is amniocentesis the only robust method to analyze fetal cells or amniotic fluid for abnormal markers. Minimally-invasive biopsy procedures performed under ultrasound guidance are available now that yield highly accurate results with minimal complications. Genetic counseling and testing options have also expanded in scope. All these improvements in prenatal testing have empowered physicians with more effective ways to detect spinal bifida early in pregnancy even before outward symptoms emerge. This plays a pivotal role in timely intervention planning and management of potentially life-threatening conditions.
Market Driver - Growing Number of Fetal Surgeries and Improved Surgical Outcomes
The success of groundbreaking fetal surgeries conducted over last two decades for severe forms of spinal bifida has significantly boosted the morale of expecting parents and healthcare professionals alike. While the first such procedure took place in the 90s, several clinical studies since then have consistently demonstrated the benefits of repairing the spinal defect in-utero rather than after birth. Two landmark trials in particular, MOMS and Management of Myelomeningocele Study or MMST, established fetal surgery as a viable treatment approach with long term neurodevelopmental advantages for children.
Spurred by these revolutionary outcomes, fetal treatment centers equipped with high-risk obstetric and pediatric surgical capabilities have been expanding worldwide. Leading medical institutions in North America, Europe and certain parts of Asia have actively started offering fetal myelomeningocele repair as a standard care option if the pregnancy meets selection criteria. For conditions where prenatal correction yields the best chance for improved mobility and reduced neurological disabilities post-birth, more expectant parents are opting for this pathbreaking intrauterine approach compared to conventional postnatal repair.
Furthermore, driven by steadily accumulating surgical experience and knowledge, the risks associated with fetal surgery itself have declined over the past decade. Refined techniques, meticulous protocolized care practices and multidisciplinary team approach help minimize preterm birth and other potential complications. As a result, more expecting mothers are agreeing to undergo the procedure knowing the benefits likely outweigh the inherent but lower risks now than before. This growing confidence in fetal surgery outcomes continues attracting larger patient volumes seeking prenatal treatment for their child's spinal bifida.
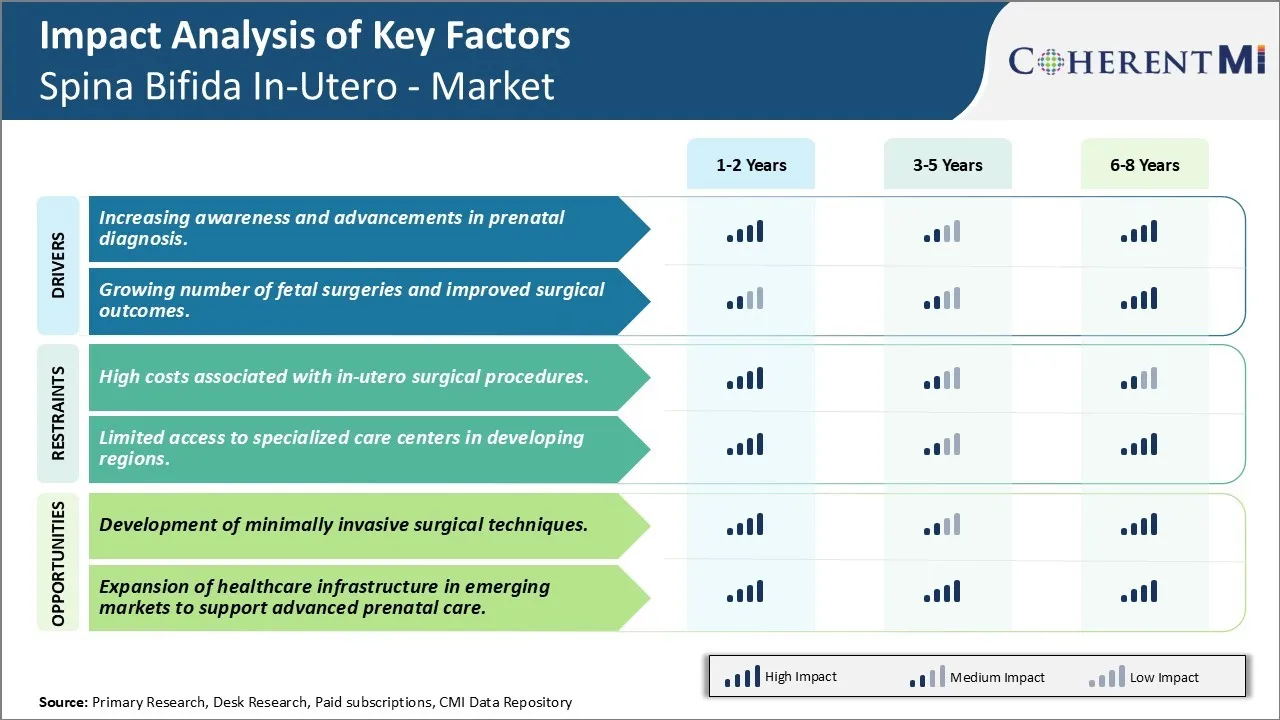
Market Challenge - High Costs Associated with In-Utero Surgical Procedures.
One of the key challenges the Spina Bifida In-Utero market faces is the high costs associated with in-utero surgical procedures to treat Spina Bifida. Such procedures require specialized fetal surgery skills and equipment as well as dedicated fetal surgery centers that can manage complex pregnancies. This level of highly specialized care comes at a significant cost. The costs of training fetal surgeons, setting up dedicated fetal surgery centers, acquiring specialized equipment like intrauterine ultrasound probes and operating microscopes, and providing round-the-clock postoperative care increase the financial burden and make these procedures unaffordable. Additionally, costs of pre- and post-surgery care and long-term management also add to the overall treatment expense. In the absence of particular measures to subsidize or reduce these costs, it will limit access to and uptake of these potentially life-changing fetal surgeries.
Market Opportunity- Development of Minimally Invasive Surgical Techniques Creates Novel Opportunities.
One major opportunity area for the Spina Bifida In-Utero market is the development of minimally invasive surgical techniques. Currently, open fetal surgical procedures require making an incision in the uterus as well as hysterotomy, which carry risks of uterine rupture in future pregnancies and premature deliveries. The adoption of advanced technology enabled minimally invasive procedures could help address some of these risks. Ongoing research in surgical robotics, advanced intrauterine ultrasound and imaging, and flexible, steerable instruments may allow developing procedures that cause minimal fetal and uterine disruption. This can potentially make these surgeries safer for mothers and babies. With reduced procedure-related risks, more fetal surgery centers and surgeons may incorporate these techniques, and insurance payers may be convinced to provide coverage. This could significantly expand access to treatment and drive growth in the long run.